Market Insight - Complexity no deterrent to research in sleep disorders
This article was originally published in Scrip
Despite recent advances in neuroscience we still do not fully understand the fundamentals of one of our most routine actions – our need to sleep, writes Naila Shaw. What is driving industry's continued investment in this area of R&D?
The question of why we sleep has yet to be answered conclusively. There are two general schools of thought: firstly, that sleep gives the body the time it needs to recuperate from the activities of the day; and secondly, that vital physiological processes and activities occur during sleep for growth, development and general metabolic "housekeeping".
The body is "programmed" to sleep and to do so at particular times of the day. When we are awake we accumulate high levels of adenosine because the day's activities require the breakdown of ATP to release cellular energy. High levels of adenosine are thought to be a major cause of feelings of drowsiness. As such they have been linked to jet lag.
The cycles of biological processes that occur between sleep give rise to the "circadian rhythm". This is largely regulated by a small group of cells called the suprachiasmatic nucleus (SCN), often referred to as the internal biological clock. The SCN is located in the hypothalamus, just above the crossing of the optic nerves. When light stimulates the photoreceptors in the retina, signals are carried back to the SCN, as well as other regions of the brain.
At particularly low levels of light, the signals received by the SCN travel to the pineal gland, which stimulates the secretion of melatonin, causing the onset of sleep. During sleep the circadian rhythms induce the heart and breathing rates to decrease and the secretion of growth hormones, melatonin and cortisol.
Researchers such as Jim Horne of Loughborough University in the UK and Dr Michael Jouvet of Claude Bernard University in France have shown that the brain uses sleep to sort information gathered from the day to file in long-term memory. They also believe that sleep is essential to maintaining normal levels of cognitive skills including speech. It has been reported that hormones which stimulate tissue and bone growth are released in larger doses during slow-wave sleep (SWS).
deprivation leads to dysfunction
One of the most common techniques for studying sleep is to observe the effects of sleep deprivation. When someone is deprived of sleep, they experience increasing mental and physical fatigue, often becoming irritable, groggy and forgetful. Sleep deprivation studies, headed by researchers at the University of Chicago, have found that severe lack of sleep has associations with the inability to metabolise glucose. As hormones and chemicals controlling appetite and weight gain are released during sleep, lack of sleep can potentially lead to conditions such as type 2 diabetes and obesity.
Further studies have also revealed that sleep deprivation interferes with many other processes including wound healing, cognitive function, growth and other day-to-day activities. Patients and volunteers in sleep deprivation studies at the UCSD School of Medicine, for example, experienced a range of symptoms including hallucinations, hypertension, paralysis, delirium, depression and weakened immune systems.
Narcolepsy, classified as excessive daytime sleepiness, is a sleep-related disorder affecting one in every 2,000 people. It is characterised by the sudden onset of muscle weakness (sleep paralysis) and the induction of sleep at unintended times, often due to strong emotions. This condition is associated with the ineffective control of rapid eye movement (REM) sleep.
Another common disorder is sleep apnoea, characterised by interruptions in breathing during sleep. It is estimated to affect one in 15 of the population. In this condition, the muscles of the throat relax, obstructing the airways, and causing one or more breaths to be missed. Sleep apnoea can potentially prove fatal, and it often remains undiagnosed for years, with the patient unaware of the sleep disturbance and becoming used to the daytime fatigue that results.
Sleep apnoea is often linked to obesity, so a great deal of success can be achieved by treating this risk factor. The most common method is known as "continuous positive airway pressure", which involves using a mask during sleep. This pushes pressurised air into the lungs, effectively forcing the airways to stay open.
Periodic limb movement disorders (PLMD), such as restless leg syndrome (RLS), are sleep-related disorders characterised by repetitive cramping or jerking of the legs during sleep, interrupting sleep and leading to sleepiness during the day. RLS differs from PLMD (although 80% of RLS patients have PLMD) due to the patient's experience of strange and uncomfortable sensations in their limbs resulting in an uncontrollable urge to move, stretch or shake their arms or legs. This condition has associations with Parkinson's disease, iron deficiency, diabetes, rheumatoid arthritis and sleep apnoea, and affects 5-10% of adults in western countries.
pharmacological intervention
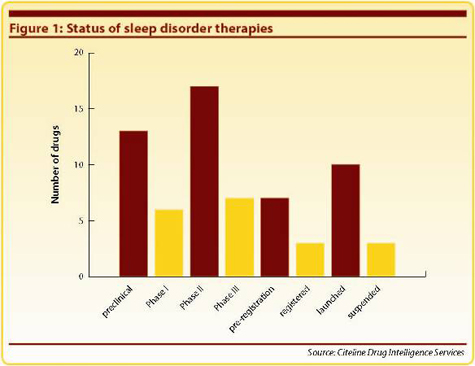
Although the past decade has seen a steady increase in the number of drugs in development for sleep disorders, there are still relatively few drugs approved or launched. Pharmaprojects' data indicate just 13 drugs registered or launched, with 43 potential drugs still in preclinical/clinical testing, and a further seven awaiting approval (see Figure 1). In pharmacological terms, nonbenzodiazepine hypnotics, dopamine D2 antagonists and orexin antagonists seem to be emerging as the front-runners in this field (see Figure 2).
Among the better known and established treatments for narcolepsy is Cephalon's modafinil, a psychostimulant first launched in France in 1994 as Modiodal for the treatment of hypersomnia and Gelineau's syndrome. It has since been launched in numerous markets for the treatment of narcolepsy. (In a US Phase III trial in 273 narcolepsy patients, once-daily treatment with modafinil for nine weeks increased wakefulness by up to 50% compared with placebo.)
A more recent addition is Jazz Pharmaceuticals' dopaminergic antagonist, Xyrem (sodium oxybate), which was first launched in the US in 2002. This drug undergoes metabolism to gamma hydroxybutyrate (GHB), thereby inhibiting presynaptic dopamine release. It is now launched in several markets for the treatment of narcolepsy-related cataplexy. In a Phase III trial in narcolepsy patients, 4.5-9.0g of sodium oxybate reduced inadvertent daytime naps and night-time awakenings, and was effective in reducing cataplectic attacks at all doses tested. Xyrem is licensed to UCB and Valeant Pharmaceuticals in Europe and Canada, respectively.
Another Cephalon compound showing future promise is armodafinil, the R-isomeric form of modafinil, which boasts an extended duration of action. In Phase III trials in Australia, Canada, Europe and the US in 300 patients, 150mg and 250mg per day of armodafinil met all the primary endpoints of objective sleep latency and was generally well tolerated. Armodafinil is approved in the US for the treatment of excessive daytime sleepiness associated with narcolepsy, sleep apnoea and shift-work sleep disorder, with launch expected in the second half of 2009.
Ramelteon, meanwhile, is a melatonin receptor antagonist, developed by Takeda for the treatment of insomnia, sleep apnoea and other sleep disorders. It is marketed in the US as Rozerem for the treatment of insomnia, and awaiting approval in Japan. A European MAA for the treatment of insomnia was withdrawn following a negative opinion from the EU's CHMP. In a Phase III trial in elderly patients with chronic insomnia, ramelteon reduced time to falling asleep, with no rebound insomnia or withdrawal observed. In a Phase II trial in sleep apnoea patients, ramelteon increased oxygen saturation in REM sleep compared with placebo. It is also in a Phase II trial for circadian rhythm sleep disorders.
And in the field of RLS, GlaxoSmithKline markets its oral dopamine D2 receptor agonist ropinirole in several countries. In a US randomised Phase III trial in 380 patients with idiopathic RLS, ropinirole significantly improved IRLS scores compared with placebo, while improving measurements of subjective sleep disturbance, sleep quality and daytime somnolence. It is also launched for the treatment of Parkinson's disease, highlighting the similarities in pathology underlying these conditions.
new avenues
Looking at novel pharmacologies as yet untested in sleep disorders, the histamine-3 receptor is under investigation as a possible target for treatment of narcolepsy. GlaxoSmithKline's 189254, which was originally in development for Alzheimer's disease, showed high affinity for H3 receptors in the cerebral cortex, and produced dose-dependent increases in levels of acetylcholine, dopamine and noradrenaline. This compound is currently undergoing Phase II trials in narcolepsy, while Johnson & Johnson's JNJ- 28583867, which showed in vivo activity at H3 receptors, and increased extracortical levels of 5-HT, dopamine and noradrenaline, is under preclinical investigation for the treatment of cognitive disorders.
Almorexant is an orexin receptor antagonist, under development by Actelion. It is in a Phase III trial in 670 primary insomnia patients to assess efficacy of 100mg and 200mg oral doses, as well as safety and tolerability. Results are expected this year. It has also shown positive results in a Phase II trial in 39 insomnia patients, where it demonstrated a significant improvement in sleep efficiency, with no adverse events or safety concerns. GlaxoSmithKline has co-development and commercialisation rights (excluding Japan) to almorexant, with Actelion eligible to receive up-front and milestone payments.
Jazz Pharmaceuticals is developing JZP-7, a transdermal formulation of ropinirole for the treatment of RLS. It is licensed to Antares Pharma, using its ATD delivery technology, and is currently in Phase II trials. In Phase I pharmacokinetic studies, JZP-7 was found to be safe and well tolerated, and achieved dose-escalation to higher doses. Phase III trials are expected in 2009, with an NDA filing and subsequent launch planned for 2011 and 2012, respectively.
An early-stage compound in the treatment of sleep apnoea is PPI-03306, under development by Biovail (Prestwick Pharmaceuticals before the acquisition). It modulates an enzyme involved in the synthesis of 5-HT. Biovail has exclusive development and commercialisation rights to PPI- 03306 for the treatment of sleep apnoea and other conditions.
conscious endeavour
After more than 50 years of research, initiated by the pioneering work of Drs Nathaniel Kleitman and Eugene Aserinsky, who in 1953 discovered REM during sleep, still relatively little is known or understood about the physiological function and importance of sleep. This line of research has, and still does, suffer from an inability to create suitable models on which to base research. The sleeping behaviours of other mammals are quite different from that of humans.
Modern sleep research is highly diverse, covering many different and overlapping areas, such as circadian neurobiology, sleep and pain, cancer and sleep disorders. New efforts may yield answers to an array of perplexing questions regarding the physiology, evolution, control and need for sleep. These answers could help to improve the diagnosis, management and treatment of sleep disorders, and could help to improve our general well being, sleep behaviour and mental health. As the conscious efforts of those in the field of sleep research and drug development continue, the near future may indeed uncover these mysteries of the unconscious.
Naila Shaw is an editorial assistant for Citeline. Email: [email protected].